
Implant-based Breast Reconstruction in New York City
Introduction to Implant-based Breast Reconstruction
At our boutique plastic surgery practice in New York City, implant-based breast reconstruction is a common procedure. Breast implants are commonly used in both aesthetic and reconstructive plastic surgery. In cosmetic surgery, breast implants are used to enlarge and/or lift the breasts. In reconstructive surgery, breast implants are used to recreate the breast mound after mastectomy. Multiple types of breast implants can be used, and breast implants can be placed either underneath or above the chest wall muscles. Over time, whether they are used for cosmetic or reconstructive purposes, all breast implants may need to be changed or removed.
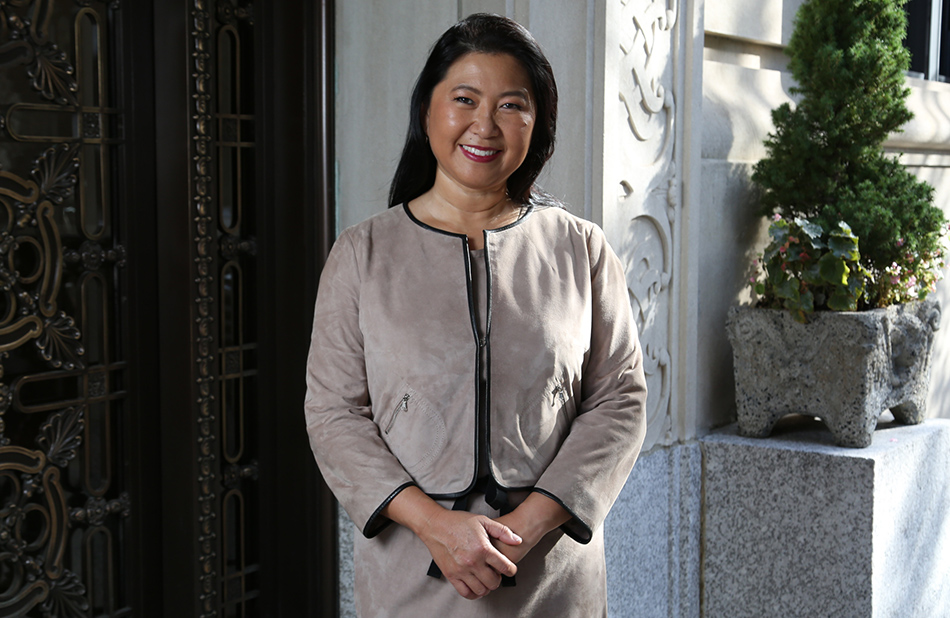
As one of the leading breast reconstruction practices in New York, Dr. Constance Chen takes pride in providing her patients with restorative options for breast reconstruction. If after reading our guide to the surgery you have questions or would like to schedule a consultation, please contact us today.
What is Implant-based Breast Reconstruction?
Implant-based breast reconstruction uses breast implants to reconstruct the breasts after mastectomy. After a patient undergoes a mastectomy, the breast is removed. For patients who would like to reconstruct their breasts, one option is to use breast implants to build a breast mound. Usually, a tissue expander is placed first – either under or above the pectoralis muscle. The tissue expander may be partially filled with air or saline, and it may be expanded after surgery in the surgeon’s office. Once the tissue expander has been completely expanded, it is exchanged for a permanent breast implant. Breast implants can have a smooth or textured shell, round or shaped, and they can be filled with saline or silicone.
Who are the Best Candidates for Implant-based Breast Reconstruction?
The best candidates for implant-based breast reconstruction are:
- Healthy with no medical comorbidities
- No need for radiation therapy
- Ideal body weight
- Non-smoker
How to Decide Between Breast Implant Types?
Breast implants may be differentiated by:

Breast Implant Filling Types
There are three different filling types for breast implants: saline, silicone gel, and cohesive gel. All three types of breast implants can be used for breast augmentation or breast reconstruction. The choice of filling is largely based on personal preference.
There are three different filling types for breast implants: saline, silicone gel, and cohesive gel. All three types of breast implants can be used for breast augmentation or breast reconstruction. The choice of filling is largely based on personal preference.
Saline – Patients who choose saline implants tend to do so because they feel confident knowing that if the implant ruptures the saline that leaks into the body’s tissues are safe. Saline is basically salt water, and it has many uses in medicine. Saline is often used to clean wounds, remove contact lenses, and help with dry eyes. Saline is injected into veins to treat dehydration, and it is also used to dilute other medications used intravenously. If a saline implant ruptures, the saline that spills into the breast tissue will be absorbed easily by the body. It will also be obvious that the implant is ruptured, as the breast with the ruptured saline implant will appear deflated.
On the other hand, saline implants are usually overfilled to make them last longer, which makes them feel more firm. Some people feel that the firmer feel makes the breast implant feel less natural. Underfilled saline implants will have wrinkles, and those wrinkles are weak spots on the implants that can lead to rupture. The firmness of a saline implant will be particularly evident in women who have little or no breast tissue.
Silicone Gel – Patients choose silicone gel implants because they want soft breasts that feel natural. Traditional silicone gel implants are prefilled with silicone gel, which is a thick, sticky fluid that is designed to imitate the feel of human fat. Silicone implants are usually underfilled, which makes them more pliable than saline implants. For this reason, patients who choose silicone implants usually do so because they believe the silicone looks and feels more like normal breast tissue.
On the other hand, silicone gel can be a problem if the implant ruptures. In 1992, all breast implants were taken off the market due to fears that they could be linked to cancer, autoimmune, and connective tissue disorders such as lupus. In 2006, after extensive studies, the FDA approved the use of silicone implants again when definitive links between silicone implants and cancer, autoimmune, and connective tissue disorders could not be firmly established. If a silicone implant ruptures, however, it is usually silent. Any free silicone tends to remain trapped in the patient’s tissues, and the rupture may not be noticeable, or else it presents as pain and discomfort. Instead of deflating, a breast with a silicone implant rupture may actually become bigger due to the inflammation that the silicone causes to any surrounding breast tissue. For this reason, the FDA recommends that women with silicone implants undergo breast MRI surveillance 3 years after implantation and then every 2 years after that.
Silicone is supposed to be inert, but it can cause irritation to the tissues if the silicone gel leaks. Sometimes the only sign of rupture is a little pain or discomfort on the side of the ruptured silicone implant. Women with silicone implants who have discomfort should undergo breast MRI to evaluate for a potential silicone implant leak.
Cohesive Gel – The newest type of breast implant is the cohesive silicone gel implant, or the “gummy bear” breast implant, which was approved by the FDA in 2012. Since the silicone in the new cohesive silicone gel implants is more cohesive than the silicone in traditional silicone gel implants, it is believed that the cohesive gel will hold together if the outer silicone shell ruptures – much like a gummy bear.
The cohesive gel implant is softer than a saline implant but firmer than the traditional silicone gel implant. Since the silicone gel is more cohesive, the cohesive gel implant tends to hold its shape because it is stiffer than traditional silicone gel. The cohesive gel implant will require the largest incision on the breast because cohesive gel implants are less flexible than all other implant types and cannot squeeze through a small incision.
Breast Implant Outer Textures
All breast implants have an outer silicone shell. The outer silicone shell in breast implants comes in two different textures: smooth and textured.
When the outer shell is smooth, the breast implant can more easily move or spin in the breast pocket. Smooth implants are less prone to infection because there are no irregular crevices for the bacteria to hide. For patients with very little or no breast tissue, smooth implants minimize the risk of visible rippling because the breast tissue cannot attach to the smooth surface. Smooth implants are more likely to develop capsular contracture, however. Over time, the slick capsule that forms around a smooth implant can shrink and contract, leading to a capsular contracture that is hard and painful.
When the outer shell is textured, the breast tissue can grow onto the surface of the implant. This allows the implant to scar in place so that it does not move around in the breast pocket. While a capsule will form around all implants, textured implants may reduce the risk of capsular contracture. Textured implants do have a slightly increased risk of infection, however, and textured implants also increase the risk of rippling in women with minimal or no breast tissue since the implant is very adherent to the breast tissue and skin.
Breast Implant Shape
Implants can be either round or teardrop shaped. Round implants are basically circles, and the circular implants can project to different heights from the chest wall. The higher the projection, the farther the breast will stick out from the chest wall. Round implants are usually smooth because if the implant moves or spins it does not change the shape of the implant. Teardrop-shaped implants have less projection at the top of the breast and more projection at the bottom of the breast, much like a natural breast. Teardrop-shaped implants should always be textured because if the implant were to move due to a smooth slippery surface the breast would appear misshapen. Cohesive gel implants are generally textured teardrop-shaped implants because they retain their shape and it is believed that maintaining a teardrop shape looks the most natural.
Breast Implant Placement
Breast implants can be placed below the pectoralis muscle or above the pectoralis muscle.
SUBPECTORAL – In both breast augmentation and breast reconstruction, breast implants are often placed under the pectoralis muscle. The advantage of placing implants underneath the pectoralis muscle is that it provides additional soft tissue coverage over the implant, which can be important when someone has very little or no breast tissue. The additional soft tissue coverage can soften the implant edges that might otherwise be visible and palpable. In addition, the action of the muscle on top of the implant can help shape the top portion of the implant so that it does not look artificially full. Finally, the squeezing action of the muscle on the implant can reduce the incidence of capsular contracture.
The action of the pectoralis muscle flexing over a breast implant can lead to hypermobility. When the muscle presses down on the implant, it can temporarily deform and change the shape of the implant and move it upward or to the side. In addition, since the pectoralis muscle is normally flat against the chest wall, the presence of an implant underneath the pectoralis muscle can feel tight or even painful. For most women, the discomfort usually improves over time, but some women never become accustomed to the tight feeling of an implant underneath the pectoralis muscle.
PREPECTORAL – Breast implants can also be placed above the pectoralis muscle, in the same location as the breast tissue. In breast augmentation, a breast implant over the pectoralis muscle is called a “subglandular” or “prepectoral” breast implant, because it is under the breast gland but over the pectoralis muscle. In breast reconstruction, a breast implant over the pectoralis muscle is just called a “prepectoral” breast implant, because it is over the pectoralis muscle but there is no glandular breast tissue after a mastectomy.
Prepectoral breast implants have the advantage of being more comfortable because there is no tightness from a foreign body being placed underneath the pectoralis muscle. There should be minimal hypermobility with the implant being deformed and displaced by the pectoralis muscle because the breast implant is over the muscle. The disadvantage is that there is not as much soft tissue coverage. Thus, it may be easier to see the outlines of the breast implant itself. This can be addressed by using a shaped implant with an acellular dermal matrix (ADM) wrapped around the implant. The ADM provides an extra layer of soft tissue coverage over the implant, and can also soften the edges of the implant itself.
Breast reconstruction with prepectoral cohesive gel implants wrapped in ADM is the newest type of implant-based breast reconstruction. ADM is composed of the dermal layer of skin that has been stripped of reactive cell components but retains the biologic qualities and structure of natural collagen. ADM eventually integrates with the body and is replaced with the patient’s own tissue. Since the implant is placed above the muscle, the normal pain and tightness from a subpectoral implant are eliminated. In addition, the cohesive gel implant retains a teardrop shape underneath the thin mastectomy skin.
Implant-based Breast Reconstruction Recovery
After implant-based breast reconstruction, patients may have drains in place for 1-2 weeks or more. Drains are removed when they are draining less than 20 cc/day x 2 consecutive days. Patients should avoid heavy lifting over 5 pounds. Patients should also avoid repetitive arm movement so that the tissues can heal in place. Prepectoral or above-the-muscle breast implants are significantly more comfortable than subpectoral or below-the-muscle breast implants, so patients will likely need significantly less pain medication. Regardless, all patients are given pain medication to address any postoperative discomfort.
What are the Complications of Breast Implants?
Almost all breast implants used in the United States have a 10-year warranty. While some implants can last for decades, many implants need to be changed in a much shorter period of time. Implants are not expected to last forever. According to data gathered by implant manufacturers, about half of breast implants need to be changed within seven years. The most common reasons for implant problems include capsular contracture, rupture, and infection.
- Breast Implant Illness
- Capsular Contracture
- Rupture
- Infection
- Extrusion
- Anaplastic Large Cell Lymphoma (rare)
- Rippling
- Breast implant that has shifted position over time
Capsular Contracture
Capsular contracture is scarring that occurs around the breast implant. All breast implants – smooth, textured, round, shaped, above the muscle, below the muscle – will develop a capsule. Since implants are a foreign body, the body tries to wall off the implant by creating a capsule around it as a barrier from the implant. The capsule can be something that is soft and flimsy – like a film that is not noticeable. Or it can become firm and painful – a hard shell that feels like it shrinks and contracts over time. When an implant develops a hard, painful capsular contracture, it is not dangerous in and of itself. The discomfort, however, may lead women to want the implant and the capsule removed in its entirety.
An en bloc capsulectomy can be performed to remove the implant and the capsule in one piece. A complete en bloc capsulectomy is a painstaking and meticulous procedure that removes every bit of the capsule, including the section that may be adherent to the chest wall and ribs. A partial capsulectomy leaves pieces of the capsule in the breast pocket. The surgical dissection from an en bloc capsulectomy is an irritant to the remaining breast tissue and will stimulate fluid production from the body. After an en bloc capsulectomy, it is usually necessary to place drains to allow the fluid from the breast pocket to exit the body. If a new implant is being placed, it is usually placed in a fresh space. In other words, if the original implant was placed subpectorally, the new implant would be placed prepectorally. Conversely, if the original implant was placed prepectorally, the new implant could be placed subpectorally.
For patients who undergo implant removal and en bloc capsulectomy and who do not want an implant replaced, drains will need to be left to drain fluid in for a longer period of time. The body does not like empty spaces and will try to fill the potential space with fluid. For patients who still have breast tissue, they may need a breast lift, or mastopexy, to rearrange any remaining breast tissue to recreate a breast mound. Otherwise, the stretched-out breast skin that has lost the volume from the implant may look empty, deflated, and unsightly. Some patients who do not want implants but need more volume may benefit from fat grafting to add bulk to their breast tissue. Fat grafting involves liposuction from another part of the body, processing and purifying the lipoaspirate, and then injecting the purified fat cells into the breast tissue to add volume.
For patients who have undergone mastectomies and thus have no breast tissue after implant removal and en bloc capsulectomies it is possible to undergo new breast reconstruction with implants or with their own tissue. Autologous tissue breast reconstruction after a mastectomy is best performed with flaps, in which skin and fat from another part of the body are transferred to the chest with its own blood supply to create a new breast. The gold standard in autologous tissue breast reconstruction is perforator flaps.
Anaplastic Lage Cell Lymphoma
In 2016, the World Health Organization determined that there was an association between breast implants and anaplastic large cell lymphoma (ALCL). ALCL is a rare type of non-Hodgkin lymphoma (NHL), cancer involving the cells of the immune system. The latest statistics on Breast Implant Associated-Anaplastic Large Cell Lymphoma (BIA-ALCL) places the incidence as approximately 1 in 450 women with textured breast implants or 0.2% of women with textured breast implants. The pathognomonic signs of BIA-ALCL are a capsular mass and/or fluid around the breast implant, with CD40 markers on pathologic or cytologic analysis indicating ALCL. For early stages of BIA-ALCL, removal of the breast implant with complete en bloc capsulectomy is curative. For more advanced stages of BIA-ALCL, chemotherapy or radiation therapy may be necessary. Worldwide, 35 patients have died of BIA-ALCL.
BIA-ALCL is extremely rare, and it is not a breast cancer but instead, it is a cancer of the scar tissue or capsule around the breast implant. Thus, women with breast implants may have a very small but increased risk of developing ALCL in the scar capsule surrounding the breast implant. There is currently no trend of implant type (saline vs silicone) or implant reason (aesthetic augmentation vs reconstruction) associated with a smaller or greater risk of ALCL. 91% of BIA-ALCL cases were in textured breast implants made by Allergan, which were taken off the market worldwide in 2019. There have been rare reports of BIA-ALCL in smooth breast implants, however. When ALCL occurs with breast implants, it is identified most frequently in patients undergoing implant revisions for late-onset, persistent seroma, which is a fluid collection that develops around the implant. Thus, the FDA does not currently recommend prophylactic breast implant removal in patients without symptoms or other abnormalities.
Rupture
Both saline and silicone implants can rupture. All implants – even saline implants – have a silicone shell, and the silicone shell can wear out over time. When a saline implant ruptures, it is quite obvious as the implant simply deflates. Since saline is the same fluid that is used intravenously to rehydrate the body, any saline that spills into the tissues should be safe. When a silicone implant ruptures, however, it is more problematic. Silicone is supposed to be inert, but the ruptured silicone gel can cause irritation and inflammation to the surrounding breast tissue that can worsen over time. Furthermore, silicone implant ruptures are usually silent so that the patient does not know that the silicone implant has ruptured. For this reason, the FDA recommends that any patient with silicone implants undergo surveillance with breast MRIs every 2-3 years.
Both ruptured saline and silicone breast implants should be removed and/or replaced. In the operating room, removing a ruptured saline implant is relatively straightforward. Removing a ruptured silicone implant, however, is more challenging because the thick sticky gel can be difficult if not impossible to remove completely. If the silicone gel spills into the tissues, it may be necessary to resect some breast tissue. This can leave breasts appearing dimpled, wrinkled, sagging, and otherwise deformed, and the remaining breast tissue may not return to its original shape. If a ruptured silicone implant is replaced, there may be a higher risk of complications compared to the first time. If an implant is not replaced, it may be necessary to perform other procedures to recreate a breast shape.
INFECTION – Since breast implants are a foreign body, they do not have a blood supply. If a patient develops breast infection, the implant cannot bring white blood cells and other natural defenders of the body to fight the infection. If the infection is a skin infection only, such as redness from cellulitis, then it may be possible to control the infection with antibiotics. If a breast implant itself becomes infected, however, because bacteria is seeded on the implant, then it needs to be removed.
EXTRUSION – Since breast implants are a foreign body, they can create pressure against the breast skin from the inside. This constant pressure occasionally leads to erosion of the breast skin so that the implant starts to push through the skin. When the breast implant pushes through the skin to the outside world, this is called extrusion. Although rare, extrusion is most common among women who have undergone radiation treatment for cancer. This is because radiation therapy damages the skin, and makes it more difficult to heal. Extrusion can also occur in breasts that have not undergone radiation if the patient or her skin has been otherwise compromised.
Nipple Reconstruction
For patients who undergo traditional mastectomies that remove the nipple-areola complex, it is possible to reconstruct the nipple. This is usually done by manipulating the remaining breast skin to create a 3-dimensional nipple. It is safest to perform a nipple reconstruction on patients who have undergone autologous tissue breast reconstruction because the breast skin will be living off of the natural tissue within it. It may not be possible to reconstruct the nipple in patients who have undergone implant-based breast reconstruction with radiation therapy, because the skin may be too compromised by radiation and the underlying artificial implant does not help keep the skin alive. In patients who cannot undergo nipple reconstruction, it is usually possible to either undergo nipple tattooing or use a 3-dimensional silicone nipple prosthesis that is attached to the breast skin with skin adhesive.
Summary of Implant-based Breast Reconstruction
Breast implants are commonly used for both aesthetic breast augmentation and breast reconstruction. Both saline and silicone breast implants have undergone extensive studies, and are currently approved for use in the USA. Breast implants are not without problems, however, and careful consideration should be given to the risks prior to placing breast implants. The FDA recently added a black box warning to breast implants, and patients are legally required to sign an extensive checklist acknowledging the risks associated with breast implants. Patients should also know that breast implants are not expected to last forever, and they may need to be removed or replaced over time.
Why Choose Dr. Chen for Implant-Based Breast Reconstruction
Dr. Chen is well-known for her expertise in breast reconstruction, including Implant-based Breast Reconstruction. She is a pioneer in the most innovative forms of breast reconstruction, including prepectoral breast implants in breast reconstruction. Dr. Chen also focuses on an aesthetic approach to breast reconstruction, because she understands the new breasts will affect a woman for the rest of her life. Some of Dr. Chen’s former patients have been so transformed by their breast reconstruction that they took the initiative to form a network, called the “Bosom Buddies,” in which they provide support and practical tips to new patients who are starting their own breast reconstruction journey.
How Much Does Implant-Based Breast Reconstruction Cost in NYC?
Implant-based breast reconstruction is covered by insurance, but an individual’s insurance benefits will vary depending on the carrier. A personal consultation is necessary in order to develop a surgical plan. Once a surgical plan is developed, our patient coordinator can provide you with a cost estimate and discuss insurance options with you.
Schedule Your Consultation
Dr. Constance Chen is well known for natural tissue breast reconstruction, and many patients fly in to New York to undergo these procedures. Please contact us to schedule a consultation. Dr. Chen looks forward to meeting with you to learn more about your situation and answer your questions.
Reach out to us

