
Breast Implant Removal in New York City
Introduction to Limited-Scar Breast Implant Removal
At our state-of-the-art practice in New York City, Dr. Chen has 20 years of expertise in performing breast implant removal through a limited scar technique. For patients who suffer from Breast Implant Illness, Dr. Chen performs an en bloc capsulectomy through an incision limited to the patient’s existing scar. Unlike most surgeons who extend the preexisting scar, Dr. Chen’s limited-scar en bloc capsulectomy removes the entire breast implant and capsule in one piece without extending the original scar.
What is Breast Implant Removal?
Breast Implant Removal surgery removes unwanted breast implants from patients who have had breast implants placed for either breast augmentation or breast reconstruction. Dr. Chen removes breast implants with a complete en bloc capsulectomy, in which all of the capsule – or scar tissue – around the breast implant is also removed.

Why Remove Breast Implants?
Almost all breast implants used in the United States have a 10-year warranty. While some implants can last for decades, many implants need to be changed in a much shorter period of time. Implants are not expected to last forever. According to data gathered by implant manufacturers, about half of breast implants need to be changed within seven years. Common reasons for breast implant removal include capsular contracture, rupture, infection, malposition, extrusion, Breast Implant Illness (BII), and cancers such as Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL) or Breast Implant-Associated Squamous Cell Carcinoma (BIA-SCC).
What is Capsular Contracture?
All breast implants heal with scar tissue encasing them, and the scar tissue wrapping around the breast implant is called the breast implant capsule. The capsule forms because the human body is trying to create a barrier to protect itself from the foreign body (ie. the breast implant). Scar tissue that forms after the placement of an implant can be soft or it can harden, causing significant discomfort. Over time, the breast implant capsule can shrink and contract, causing painful capsular contracture. In addition, the breast implant capsule is not impermeable, and heavy metals, silicone, and other substances can leak through from the breast implant shell. Capsular contracture is one of the most common reasons to have the implants and scar tissue removed.
What is Breast Implant Rupture?
All breast implants are made with a silicone shell, which can wear out over time. The silicone breast implant shell is either filled with saline – the same salt water that is used in intravenous fluids – or silicone. Both saline and silicone implants can rupture. When a saline implant ruptures, it is usually obvious as the implant simply deflates, and the breast appears smaller and deflated. In addition, the saline that spills into the tissues is considered safe, as saline is the same fluid that is used intravenously to rehydrate the body or in contact lens solution. When a silicone implant ruptures, however, it is usually silent and the patient may not realize it. Silicone is supposed to be inert, but the ruptured silicone gel can leak out and cause irritation to the surrounding breast tissue. Instead of deflating the breast, as a silicone leak progresses a ruptured silicone implant can actually lead to the breast growing larger due to inflammation of the surrounding breast tissues.
Both ruptured saline and silicone breast implants should be removed and/or replaced. In the operating room, removing a ruptured saline implant is relatively straightforward. Removing a ruptured silicone implant, however, is more challenging because the thick sticky gel can be difficult or even impossible to remove entirely. If the silicone gel spills into the tissues, it may be necessary to resect some breast tissue. This can leave breasts appearing dimpled, wrinkled, sagging, and otherwise deformed, and the remaining breast tissue may not return to its original shape. Over the years, Dr. Chen has developed a meticulous technique to remove the spilled silicone gel while preserving as much breast tissue as possible in order to avoid/reduce postoperative changes. If a ruptured silicone implant is replaced, there may be a higher risk of complications compared to the first time. Sometimes, it’s safer to avoid replacing the implant immediately to minimize the risk of infection. If an implant is ultimately not replaced, however, it is sometimes necessary to perform other procedures to recreate the breast shape.
What is Breast Implant Infection?
Breast implants are at higher risk for infection than living breast tissue without breast implants because implants are a foreign body without a blood supply. If the breast or breast implant becomes exposed to bacteria, the implant cannot bring white blood cells and other natural defenders of the body to fight the infection. If the breast with a breast implant infection is limited to the skin only, such as redness from cellulitis, then it may be possible to control the infection with antibiotics. If a breast implant itself becomes infected, however, because bacteria is seeded on the implant, then it needs to be removed. An untreated infection from a breast implant can lead to systemic infections, which is the only true medical emergency associated with breast implants requiring immediate attention. Infection from breast implants can occur any time – days, years, and even decades – after the breast implant is placed. For this reason, patients with breast implants should take prophylactic antibiotics when undergoing invasive procedures such as teeth cleaning and colonoscopies to minimize risk.
What is Breast Implant Malposition?
Breast implants are placed under breast skin or muscle to either create a larger breast or to recreate a breast that has been removed. Over time, the breast implant can shift position. This is especially true if the breast implant is placed underneath the pectoralis muscle, because the action of the pectoralis muscle runs from the top of the arm near the shoulder to the middle of the chest. Every time the pectoralis muscle is flexed during arm movement the muscle can squeeze the implant into the armpit area. Gravity, weight gain, and trauma can also cause the breast implant to move over time. For patients who have breast implants placed due to a need for breast reconstruction and who also undergo radiation therapy, the breast skin will shrink over time and push the breast implant higher on the chest wall. Since breasts are intended to be a symmetrical pair, malpositioned breast implants that cause breast asymmetry may lead a woman to want their breast implants removed and/or adjusted so that her breasts appear more symmetrical.
What is Breast Implant Extrusion?
Breast implants create pressure against the breast skin from the inside. Occasionally, this constant pressure leads to erosion of the breast skin so that the implant starts to push through the skin. When the breast implant pushes through the skin, this is called extrusion. Extrusion is most common among women who have undergone radiation treatment for cancer. This is because radiation therapy damages the skin, and makes it more difficult to heal. Extrusion is not limited to radiated skin, however, and patients with thin skin and/or little breast tissue can also suffer from extrusion. Sometimes, the breast implant can push through a weak spot in an incision or healed scar. If a breast implant extrudes through the skin, it is considered contaminated no matter how clean it looks, and the breast implant needs to be removed. If the patient wants to replace the breast implant after extrusion, it is usually prudent to use a smaller size breast implant.
What is Breast Implant-Associated Squamous Cell Carcinoma?
Breast Implant-Associated Squamous Cell Carcinoma (BIA-SCC) is an even more rare but potentially aggressive epithelial-based cancer that appears to be associated with breast implants. Like BIA-ALCL, BIA-SCC also appears to come from the scar tissue around the breast implant, known as the breast implant capsule. At this time, there are so few reported cases of BIA-SCC that it is not possible to determine what factors increase patient risk. The FDA is only aware of 19 cases of BIA-SCC in the breast implant capsule.
What is Breast Implant Illness?
Breast implant Illness (BII) encompasses a constellation of autoimmune symptoms that includes chronic fatigue, brain fog, joint aches, food and drug allergies, skin and hair problems, and many other issues that affect women with breast implants. While BII is not recognized by insurance companies as a covered medical diagnosis, people who suffer from BII report developing problems after breast implants are placed; once their breast implants are removed, the symptoms resolve. Typically, people who suspect that their symptoms are due to BII have consulted with numerous healthcare practitioners who are unable to pinpoint the source of their problems despite a wide array of laboratory, radiological, and other tests. Ultimately, BII becomes a diagnosis of exclusion after all other known causes of the physical symptoms are ruled out.
While insurance companies may not recognize BII as a medical diagnosis, there have been numerous studies that show a higher association of autoimmune problems in patients with breast implants. For example, a 2019 study published by the University of Texas MD Anderson Cancer Center looked at long-term outcomes of almost 100,000 women with silicone breast implants and found up to 8 times the normal population rates of rare diseases like rheumatoid arthritis, scleroderma (a connective tissue disease), and Sjögren’s syndrome (an autoimmune disorder), as well as three to four times the incidence of stillbirth and melanoma. In 2018, an Israeli study compared 25,000 women with silicone breast implants to 100,000 women without implants and found that there was a 22 percent higher rate of risk of autoimmune or rheumatic disorders among the women with implants. While these studies do not prove a cause-and-effect relationship between breast implants and autoimmune issues, the association has caused concern among many women with breast implants – especially those whose unexplained symptoms only developed after getting breast implants. With BII, symptoms resolve almost immediately after breast implants are removed.
What is Breast Implant-Associated Anaplastic Large Cell Lymphoma?
In 2016, the World Health Organization determined that there was an association between breast implants and anaplastic large cell lymphoma (ALCL). ALCL is a rare type of non-Hodgkin lymphoma (NHL), cancer involving the cells of the immune system. Recent statistics on Breast Implant Associated-Anaplastic Large Cell Lymphoma (BIA-ALCL) places the incidence as approximately 1 in 450 women with textured breast implants or 0.2% of women with textured breast implants. The pathognomonic signs of BIA-ALCL are a capsular mass and/or fluid around the breast implant, with CD40 markers on pathologic or cytologic analysis indicating ALCL. For early stages of BIA-ALCL, removal of the breast implant with complete en bloc capsulectomy is curative. For more advanced stages of BIA-ALCL, chemotherapy or radiation therapy may be necessary. According to the United States Food & Drug Administration (US FDA), BIA-ALCL has a mortality rate of 5%. As of March 2023, 59 patients have died of BIA-ALCL worldwide.
BIA-ALCL is extremely rare, and it is not a breast cancer but instead, it is a cancer of the scar tissue or capsule around the breast implant. Thus, women with breast implants may have a very small but increased risk of developing ALCL in the scar capsule surrounding the breast implant. There is currently no trend of implant type (saline vs silicone) or implant reason (aesthetic augmentation vs reconstruction) associated with a smaller or greater risk of ALCL. 91% of BIA-ALCL cases were in textured breast implants made by Allergan, which were taken off the market worldwide in 2019. There have, however, been rare reports of BIA-ALCL in smooth breast implants. When ALCL occurs with breast implants, it is identified most frequently in patients undergoing implant revisions for late-onset, persistent seroma, which is a fluid collection that develops around the implant. ALCL can also be visualized as a capsular mass on the breast implant capsule – not in the breast tissue itself. In either case – periprosthetic fluid or a capsular mass – the fluid or mass can be biopsied to obtain a diagnosis of ALCL prior to surgery. The FDA does not currently recommend prophylactic breast implant removal in patients without symptoms or other abnormalities.
How are Breast Implants removed?
It is important that each woman understands the various procedures for removing a breast implant. Breast implants can be removed with or without some or all of the breast implant capsule. Due to concerns about BIA-ALCL and BIA-SCC, which is a cancer of the breast implant capsule, many women understandably seek to have their breast implants removed with the entire breast implant capsule. A complete capsulectomy is a time-consuming and meticulous procedure that involves removing not just the breast implant but the entire capsule that surrounds it. In some cases, this requires removing capsular material that may be attached to the chest wall or ribs, which can be adherent to the thin covering around the lungs. An en bloc capsulectomy removes the implant and the capsule in one piece, and it is considered the gold standard of breast implant removal. To save time and reduce risk of lung injury, however, many surgeons may remove only part of the capsule, leaving much of the capsular material behind, or they remove only the implant while leaving the entire capsule behind. Removal of the breast implant while leaving the entire breast implant capsule behind is usually a quick procedure, but it is insufficient to address concerns about BIA-ALCL or BIA-SCC.
There are multiple factors to be considered in breast implant removal, including thoroughness of the capsule removal (capsulectomy), operative time, scarring, and postoperative appearance. Breast implant removal with a complete en bloc capsulectomy can be challenging – particularly if the breast implant has been placed below the pectoralis muscle. When the breast implant has been placed above the pectoralis muscle, breast implant removal is a much simpler procedure because the capsule will not be adherent to the ribs. To simplify the en bloc capsulectomy, many surgeons will make a very large incision to make it easier to gain access to the implant but this will unfortunately leave a larger permanent scar. Other surgeons will forgo removing some or all of the breast implant capsule to simplify the procedure. Dr. Chen avoids enlarging the implant placement scar during the removal procedure and instead works through a patient’s existing scar to remove the entire capsule and implant.
What is Limited Scar En Bloc Capsulectomy?
Removing breast implants with a complete en bloc capsulectomy through an existing scar is unique because most surgeons will either leave behind some or all of the implant capsule or they will create a long scar to perform an en bloc capsulectomy. Unlike other surgeons who will often create a long scar to remove a woman’s breast implant, Dr. Chen avoids enlarging the implant placement scar during the removal procedure and instead works through a patient’s existing scar to remove the entire capsule and implant.

What are the Benefits of Breast Implant Removal?
If you have decided that you no longer want your breast implants, Dr. Chen can remove your breast implants with a complete en bloc capsulectomy. Some of the benefits our New York City patients have seen are:
- Better Mammogram visibility
- Resolution of pain and discomfort from breast implants
- Resolution of BII symptoms
- No need to worry about breast implant complications
- No need for MRIs for ruptures
- No fear of ruptures
- No need for replacements
- Short recovery time
What’s the First Step?
The first step in getting Breast Implant Removal in NYC with Dr. Chen is to contact our office and schedule a consultation. During this one-on-one meeting with Dr. Chen, you will be able to ask questions and discuss your personal goals. Dr. Chen will assess your needs and develop a plan with you to address your concerns.
What to Expect on the Day of Breast Implant Removal?
On the day of your surgery, you will be met by a nurse, an anesthesiologist, and Dr. Chen. Your surgery will be performed under general anesthesia so you will not feel anything during surgery.
Dr. Chen will then almost always use your current scar to remove your breast implant. In rare cases, she may need to extend your current scar if it is extremely small or make an additional incision to gain access to the breast implant. Dr. Chen will remove the implants and any scar tissue through this incision, which is then closed with dissolving sutures.
Breast Implant Removal Recovery
Once you are finished with your surgery, you will be able to return home and begin your recovery on the same day. You may be wrapped in a compressive dressing, and you should avoid heavy lifting over 5 pounds for 6-8 weeks. If you have drains, they are usually removed in the first 1-2 weeks. You will be prescribed pain medication for any postoperative discomfort.
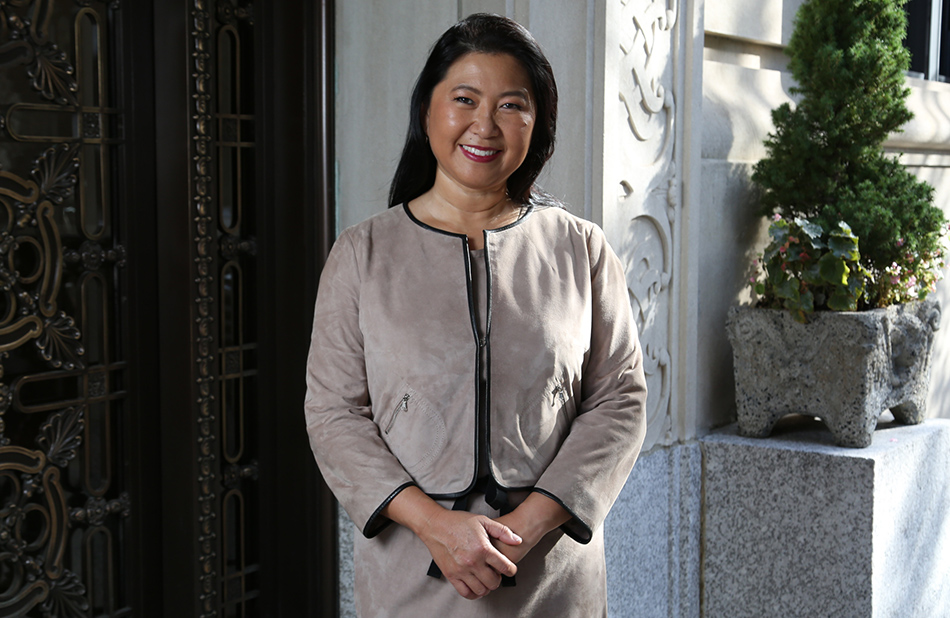
Why Choose Dr. Chen for a Breast Implant Removal
Dr. Constance Chen is a board-certified plastic surgeon with special expertise in using innovative, natural techniques to optimize medical and cosmetic outcomes for women. She understands that every woman has her unique concerns and treatment preferences, and prides herself on being able to give every patient highly individualized attention. She is experienced in removing breast implants with a complete en bloc capsulectomy – even underneath the pectoralis muscle. In addition, she is one of the few plastic surgeons who are capable of performing implant removal with a complete en bloc capsulectomy through a small incision.
How Much Does a Breast Implant Removal Cost in NYC?
The cost of Breast Implant Removal in NYC will vary from patient to patient. A consultation is necessary to formulate a surgical plan. Once a plan is determined, Dr. Chen’s staff will put together a cost estimate for you.
Schedule Your Consultation
When you feel that a Breast Implant Removal in New York City is best for you, we encourage you to contact our Manhattan office and schedule your one-on-one consultation with Dr. Chen. She looks forward to meeting with you and helping you find the comfort and aesthetic appearance you want.
REACH OUT TO USBreast Implant Removal FAQs
Is Breast Implant Removal painful?
The surgery itself is performed under general anesthesia, so there is no pain during the procedure itself. Dr. Chen usually uses a regional anesthetic in the chest wall that keeps the surgical site numb for 3-5 days. She also prescribes postoperative pain medication if there is any additional discomfort after surgery.
How many appointments will I need?
After your initial consultation, Dr. Chen will typically see you 1 month prior to surgery, 2 weeks prior to surgery, and just prior to surgery for preoperative marking. Following your surgery, Dr. Chen will have you return for some follow-up visits to ensure that your recovery is going well. Usually, she will see you 1 week after surgery, then 2 weeks, 1 month, 3 months, 6 months, and 1 year after surgery.
How long until I see results?
Patients who are removing their breast implants due to pain and discomfort will usually notice a difference immediately after surgery. That is, they will almost always notice that their symptoms have either improved or even disappeared entirely. The appearance of their breasts, however, will evolve over time. Breast Implant Removal is a surgery that can have a variety of results as swelling and postoperative changes need time to see post-operative results. The skin will contract and any remaining breast tissue will reexpand. The results also depend on the size of the implants being removed, as well as the quantity and quality of the breast tissue that is left. It can take 6 months to a year for patients to see their final aesthetic results.
Can I combine Breast Implant Removal with other procedures?
Yes, some patients combine Breast Implant Removal with a Breast Lift or fat grafting for optimal appearance. Other patients have chosen to have other cosmetic procedures such as Liposuctions, Tummy Tuck, or mommy makeovers. If you are interested in additional procedures performed, please discuss this with Dr. Chen during your consultation.
What are the risks associated with Breast Implant Removal?
As with any surgery, there are possible risks associated with breast implant removal surgery. These risks include, but are not limited to:
- Anesthesia risks
- Asymmetry
- Bleeding
- Cardiac and pulmonary complications
- Deep vein thrombosis
- Deflated, unattractive breasts
- Fatty tissue found deep in the skin might die
- Fluid accumulation
- Hematoma
- Infection
- Numbness or other changes in nipple/areola sensation
- Numbness or other changes in skin sensation
- Persistent pain
- Pneumothorax
- Poor healing of incisions
- Possibility of revision surgery
- Prolonged swelling
- Recurrent looseness of skin
- Scarring
- Skin discoloration
- Suboptimal aesthetic result
- Unfavorable scarring


